When someone is critically injured and there is a significant loss of blood, stopping the bleeding is the main priority. If you can’t stop the bleeding, their chances of survival are slim. First responders and other medical personnel train frequently on stopping bleeding in major injuries. They use bandages, tourniquets, and other medical equipment aimed at saving lives.
However, treatment doesn’t stop after the bleeding does. People who lose a large amount of blood typically go into what is called hemorrhagic shock. This type of shock is the result of an imbalance in fluids that leads to serious symptoms.
Treating hemorrhagic shock needs to happen quickly to restore proper fluid levels and keep the patient alive. Here are some ways it can be treated and how you can spot hemorrhagic shock in a patient.
Spotting Signs of Hemorrhagic Shock
For the most part, hemorrhagic shock happens in conjunction with a traumatic injury like a serious cut, burns, a gunshot, and other similar injuries. When your blood is leaving the body, your organs, brain, and other parts of your body don’t have sufficient blood supply. Your body kicks into survival mode by going into shock and shutting down certain bodily functions.
When someone goes into shock, there is usually a steep drop in blood pressure and body temperature. Left untreated, shock can be deadly.
Some of the common signs of shock, aside from low blood pressure and body temp, include things like confusion, dizziness, a weak pulse, anxiety, blue lips and fingernails, sweating, rapid shallow breathing, and other signs of distress.
Remember, not all blood loss means that blood is leaving the body. While it’s easy to spot hemorrhaging from a gunshot or a knife wound, the bleeding can also be happening inside of the body. People in a car accident, for instance, can be bleeding inside. If you see abdominal swelling, a patient throws up blood or complains of serious internal pain, it could be a sign of internal bleeding.
Treading Hemorrhagic Shock
Significant blood loss needs to be treated rapidly. In addition to making attempts at stopping the bleeding, people on the scene should call 9-1-1. When first responders arrive, they’ll be better equipped to treat the bleeding and other conditions like shock. Medical experts often recommend keeping the patient warm with a blanket until they get to a medical facility. Lay the person down and tell the patient to stay still to avoid expending more energy than necessary. Don’t let them eat or drink anything, and if they vomit, turn them on their side to prevent them from choking. Of course, only move the patient if you know there is a possible spinal injury. Moving someone with an injured spine can lead to serious health problems down the road.
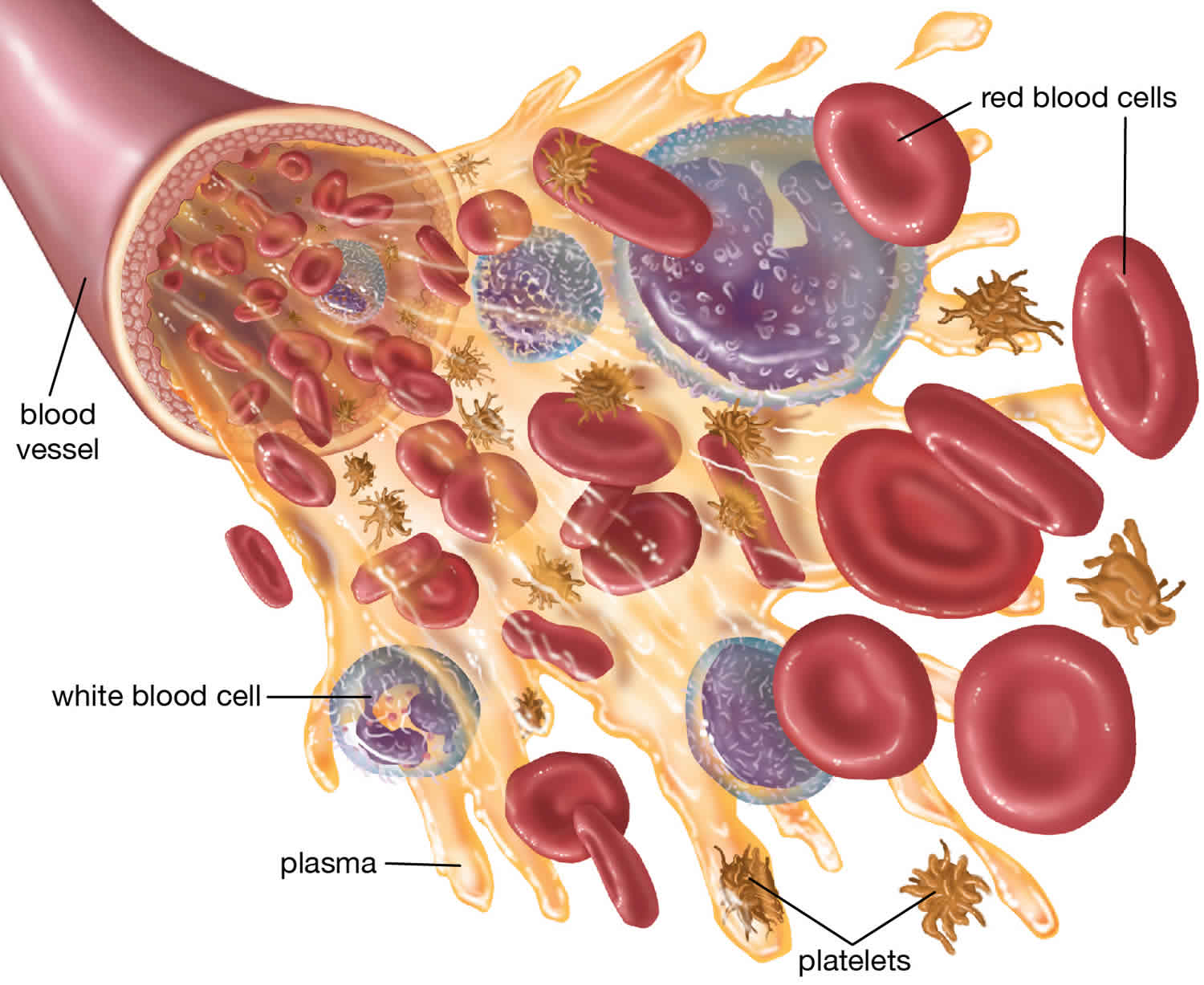
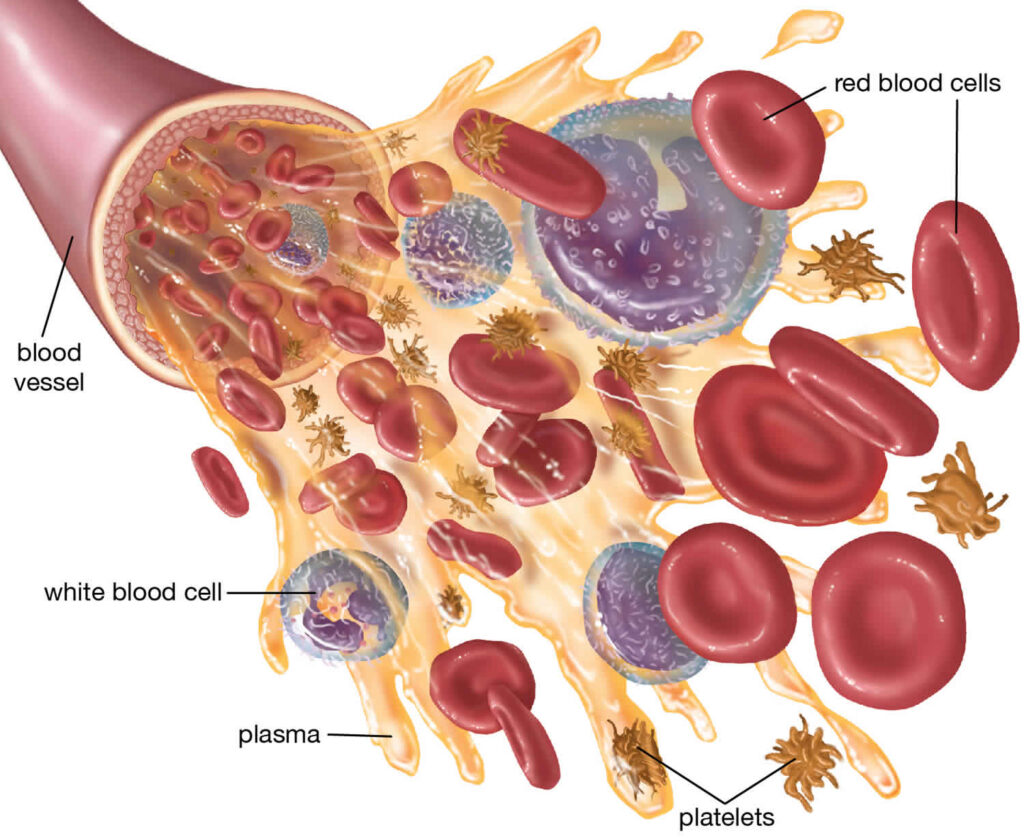
Once at a hospital, the patient will have access to advanced treatments that will manage the shock more effectively. They’ll begin the work of replenishing the body’s fluids with things like blood transfusions, IVs, and other interventions.
Peptides & Hemorrhagic Shock
PT-141 is an advanced peptide that was investigated as a treatment for acute hemorrhage in 2009. In testing trials, https://www.peptidesciences.com/pt-141-10mg was shown to protect tissues against inadequate blood supply. Currently, in phase IIl trials, the peptide has shown that it binds to MC-1R and MC-4R to reduce ischemia and low effects of shock.
Understanding the Long-Term Effects of Shock
You’re right if you think that stopping the bleeding is the most important thing to do when treating traumatic injuries. If you can’t stop the bleeding, then whether a patient goes into shock won’t matter much. You can only live for so long before too much blood loss affects the function of critical organs too greatly.
However, after the bleeding is stopped, failing to treat chock properly can have short-term and long-term negative effects on a patient. People who experience long periods of hemorrhagic shock can suffer from organ damage or failure and even death.